High Trauma Response Fees May Be Upsetting, But They Are Necessary

(Updated 7/23/2018)
Healthcare reimbursement issues are frequently misunderstood and many in the public are generally left with the impression that hospitals simply charge way too much for services they render to patients. In fact, usually when the subject of healthcare charges come up, many people cite to the anecdotal $30 aspirin as justification for their contention that there is rampant overcharging.
So when I came across this story about trauma response fees last week, I was not surprised at the biased approach taken by reporters and ‘experts’ who clearly lack the knowledge necessary to evaluate the reasonableness of healthcare charges and reimbursement. It highlights the ongoing problems healthcare providers face when there is a failure on the part of the public to understand and appreciate the real problems hospitals face when they deliver lifesaving services to the public.
What’s the story?
During 2016, an eight-month-old child of a couple on vacation from South Korea fell off the bed in their hotel room in San Francisco and hit his head.
After their baby fell, the parents could not calm him down. They did what any concerned parents in this situation would do – they called 911.
An ambulance came and took the family to Zuckerberg San Francisco General Hospital – the only Level 1 Trauma Center in San Francisco and northern San Mateo.
Luckily, at the hospital it didn’t take long for the experienced, highly skilled and well trained doctors to determine that the baby would be just fine. All he had was a little bit of bruising on his nose and forehead. After napping in his mother’s arms and drinking some infant formula, he was discharged a few hours later with a clean bill of health. The couple continued their vacation and the incident was quickly forgotten according to the story from Vox.
The total hospital visit reportedly lasted 3 hours and 22 minutes.
Two years later, the parents of this young child received a bill totaling $18,836 for his treatment. (It probably took the hospital a long time to locate them in South Korea ).
The majority of the bill, $15,666, was for “trauma activation,” also called a “trauma response fee.” “A trauma fee is the price a trauma center charges when it activates and assembles a team of medical professionals that can meet a patient with potentially serious injuries in the ER. It is billed on top of the hospital’s emergency room physician charge and procedures, equipment, and facility fees,” according to Vox.
But to truly understand what this fee is, it is necessary to understand what a Level 1 Trauma Center is. (You may recall our discussion about trauma centers earlier).
Trauma is one of the leading causes of death in the United States and a trauma center is a hospital that has been certified to treat serious life-threatening physical injury, with potential complications of shock, respiratory failure, and death.
And Zuckerberg San Francisco General Hospital is not your average trauma center. It is what is referred in the industry as a Level 1 trauma center – the best!
Level 1 trauma centers like Zuckerberg San Francisco General Hospital are usually fully staffed and equipped with highly trained personnel necessary to handle ANY traumatic event 24 hours each day and every day of the week. In other words, Zuckerberg San Francisco General Hospital and other Level 1 trauma centers have the most advanced, readily available resources and staff to treat serious life threatening injuries. (Levels 2 – 4 trauma centers are generally not as well staffed as Level 1 and when appropriate, they transfer patients to Level 1 trauma centers. There are usually relatively fewer Level 1 trauma centers compared to Levels 2-4.
The trauma activation fees, which are usually $10,000 or more, may feel like a punch in the gut not only because of their high price tags but also because sometimes it may appear to the untrained eye that they are borne by people who have undergone pretty minimal treatment.
“It’s a huge amount of money for my family,” said Jang (mother of the baby boy), whose family had travel insurance that would cover only $5,000.
“If my baby got special treatment, okay. That would be okay. But he didn’t. So why should I have to pay the bill? They did nothing for my son.”
But are these trauma response fees fair or reasonable?
Clearly, trauma hospitals require a full time team of highly skilled medical professionals who must be compensated to be on call 24/7 for medical emergencies irrespective of whether a single trauma case walks in the door.
“We are the trauma center for a very large, very densely populated area. We deal with so many traumas in this city — car accidents, mass shootings, multiple vehicle collisions,” said Brent Andrew, spokesperson for Zuckerberg San Francisco General Hospital. “It’s expensive to prepare for that.”
Andrew defended the $18,836 bill the family of the baby boy received.
Here are a few examples of what our experts here at SAC had to say about this incident and the reasonableness of the charges associated with trauma activation fees:
- If the skilled medical professionals were not immediately available to properly evaluate the baby and he actually suffered a concussion and later died as a result of not receiving proper treatment, the parents would be suing the hospital for millions of dollars.
- First, the parents should have been reported to child protection, as the baby was 8-months-old and fell off a bed. Where is the crib? Second, the baby came in with a possible concussion. That is what happens when a baby falls off a bed and hits its’ head. Medically, the baby needs to be observed for a time for possible concussion. Sorry, but the charges to have a skilled medical team always on-call for situations like these are entirely justified here.
- Does not talk about the fact that the baby lands on the forehead and nose, which would activate a pediatric neurologist and pediatric trauma physician. Also, the baby would never be able to leave without monitoring brain swelling or neuro conditions for at least 2 to 3 hours. But per the parents, they said a nap and a bottle? Good thing they had a great outcome – could have been worse.
- These articles invariably rely upon misleading and anecdotal stories. No reference to all the uncompensated care and charity care that hospitals provide. Any objective look at hospital balance sheets on a macro level shows that the margins are very tight. If hospitals are really gauging patients and raking in all this money, then why do we have so many hospitals struggling or going out of business?
- Since this story has made the rounds here at SAC this morning, permit me to add my two cents to the discussion. I read the story in its entirety. The implication of the story is that these particular cherry-picked stays’ charges were unconscionably high. This sort of complaint comes up quite often in our work, so I am going to give you a brief rundown on the hospital perspective that the writers of these type of articles never seem to include.
EVEN WITH CHARGEMASTER FEES AS HIGH AS THEY ARE, HOSPITALS DON’T MAKE MUCH OPERATING PROFITS
The article focuses on Zuckerberg San Francisco General Hospital & Trauma Center. So, let’s look at that facility’s financial numbers for 2016, which is the most current year that California’s Office of Statewide Health Planning and Development (OSHPD) has published data.
Here is the summary data regarding that facility:
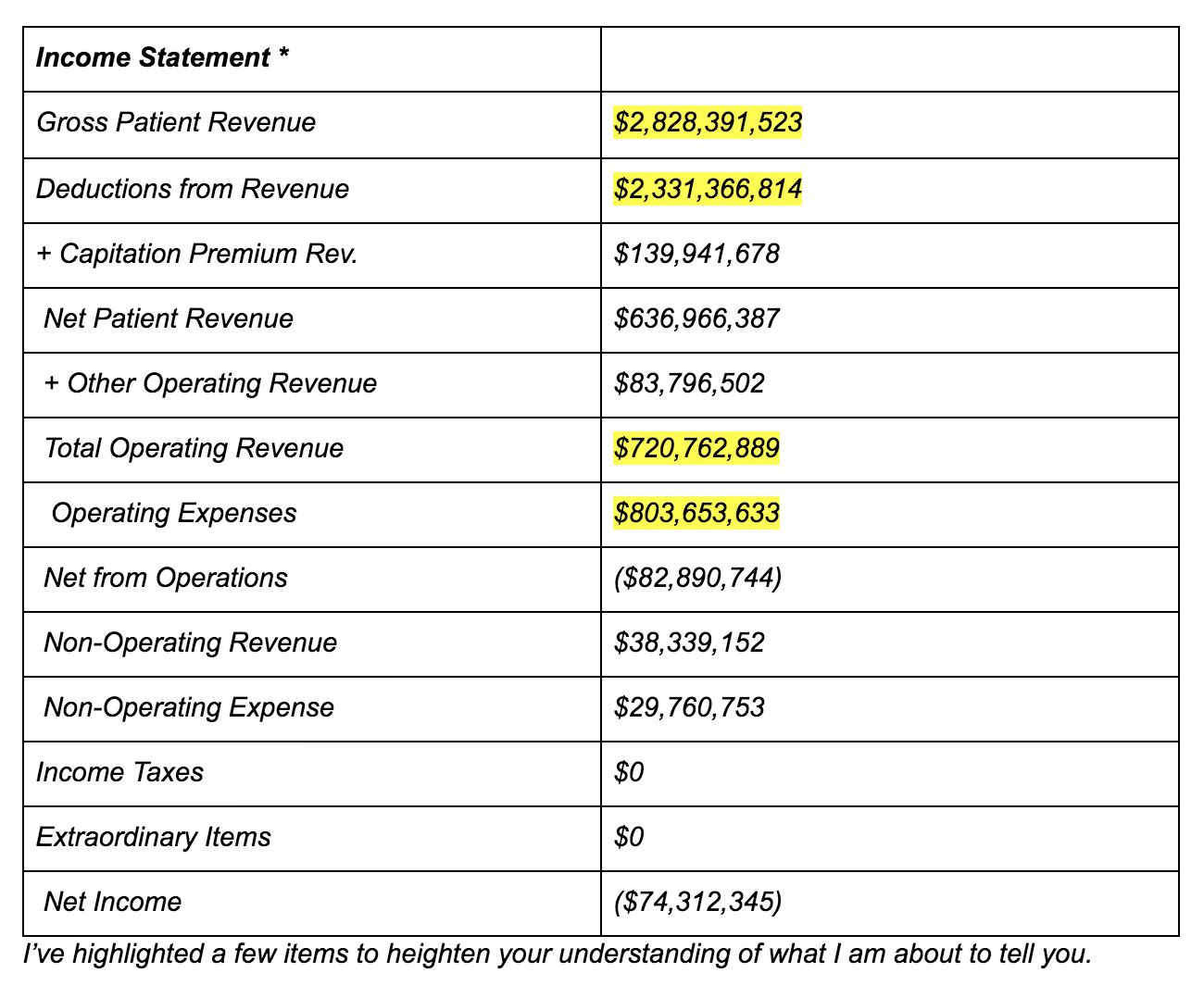 First is the Gross Patient Revenue figure of $2,828,391,523.
First is the Gross Patient Revenue figure of $2,828,391,523.
That is the sum total of all the hospital billing forms that the hospital generated in 2016. IT DOES NOT REPRESENT PAYMENTS THAT HOSPITAL RECEIVED FOR PATIENT CARE IN THAT TIME PERIOD.
Rather, it is the next highlighted figure of Total Operating Revenue of $720,762,889 that represents actual cash received by the hospital for patient care. As you can see, there is an ocean of a difference between receiving $2.8 billion vs $720 million).
To put all this as simply as possible…
The hospital charged nearly $3 Billion for patient care, but it only collected $720Million.
The next two highlighted figures are critical.
Operating Expenses of $803,653,633 is exactly what it means – that hospital paid nearly $804 Million for the care it rendered to patients for care in 2016. Those payments were for the salaries for the nurses, the janitorial staff, the admission desk workers, and the orderlies; for the electricity and heating in the operating rooms, the emergency room, and the patients’ rooms; for the bandages, implants, light bulbs, and antiseptic cleaners used to clean the rooms; etc.
Now, compare the Total Operating Revenue figure of $720,762,889 to the Operating Expenses figure of $803,653,633.
Do you see what I see?
THE HOSPITAL SPENT MORE MONEY TO CARE FOR ITS PATIENTS THAN IT RECEIVED FOR CARING FOR THOSE PATIENTS.
How much did the hospital lose? The hospital spent $82,890,744 more (i.e., the Net from Operations figure).
In other words, this particular hospital loses more money every time a new patient walks in the door (to be precise, on average of $468.25 per day for each patient).
This exercise should disabuse the notion that hospitals charge too much for its care; rather, for this hospital it is better accused of charging too little because it is running at a loss.
SOMEONE MUST PAY FOR THE TRAUMA TEAM. WHY NOT THE TRAUMA PATIENTS?
The article did not discuss the question of “what the fair way is to pay for the extra costs associated with having a first-rate trauma center if such expenses are not paid for by the trauma patients themselves?”
If you can’t charge the trauma patients, and the hospital has no money, then the only sustainable alternative would be to charge more – in other words, raise all the hospital prices for patients generally, especially for the non-trauma patients.
Well, the article has problems with that alternative as well, as evidenced by this remark:
“But that logic leaves (other patients)…with tens of thousands in potential debt for care they didn’t ask for or need . . . “
So on the one hand the article pulls your heartstrings with anecdotal cases of seemingly high hospital bills, but on the other hand it squashes any possibility for any alternative by championing the general principle that patients should not “foot the bill” for “care they didn’t ask for or need . . .,” which presumably means non-trauma patients should not pay for trauma care. In short, no one should have to pay for the trauma center.
To summarize all these SAC point of views, most hospitals do not arbitrarily determine their charges. Charges take into account various factors including the type of service and the amount of ‘free’ care that they are required to provide in order save lives and maintain the health of our communities. The government doesn’t cover all these charges. Someone has to. The services are critical and hospitals have to keep our trauma doors open. So who do you suggest should pay for these medically necessary services?
In recent news, Zuckerberg San Francisco General Hospital agreed to waive the $15,666 trauma response fee. We cannot definitely say, but perhaps this is because this case received so much media attention.
Reportedly, a patient experience manager issued “a sincere apology for any distress the family experienced over this bill.”
The hospital manager also said this whole situation “offered us an opportunity to review our system and consider changes.”